What is Azoospermia (Zero Sperm Count) ?
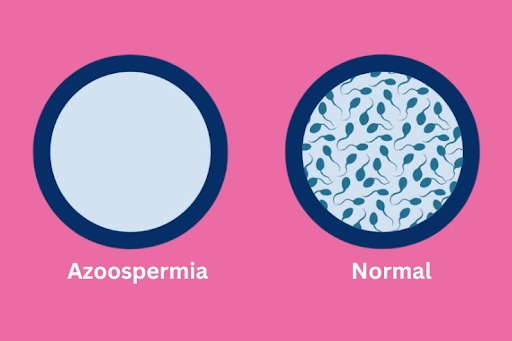
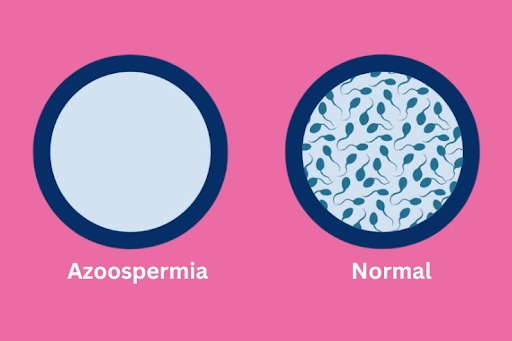
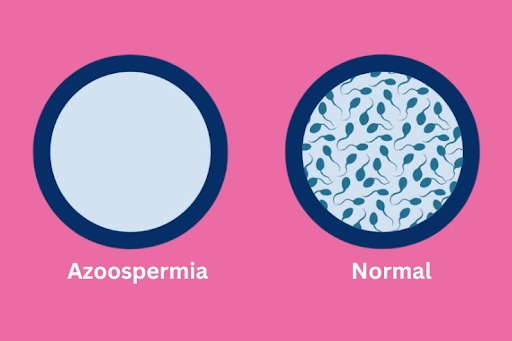
No sperm count, also known as azoospermia, is a medical condition characterized by the absence of sperm in the ejaculate. In men with azoospermia, semen analysis reveals no sperm present, making natural conception difficult or impossible without medical intervention. Azoospermia can result from various factors, including problems with sperm production in the testes, blockages in the reproductive tract preventing sperm from reaching the ejaculate, or other underlying medical conditions. Understanding azoospermia is essential for individuals and couples seeking to address fertility issues and explore available treatment options.
Types of Azoospermia (Zero Sperm Count)
Azoospermia, or no sperm count, can be classified into two main types based on its underlying cause and mechanism:
- Obstructive Azoospermia:Obstructive azoospermia occurs due to physical blockages or obstructions in the male reproductive tract, which prevent sperm from being ejaculated despite normal sperm production in the testes.
- Non-obstructive Azoospermia:Non-obstructive azoospermia is characterized by the absence of sperm in the ejaculate due to factors that impair sperm production within the testes, such as hormonal imbalances, genetic abnormalities, or testicular dysfunction.
- Pretesticular Azoospermia:Pretesticular azoospermia refers to conditions that disrupt normal sperm production by affecting hormonal signals or pathways that regulate sperm production in the testes. Examples include hypothalamic or pituitary disorders that result in hormonal imbalances.
- Testicular Azoospermia:Testicular azoospermia occurs when there is a failure of sperm production within the testes themselves, typically due to factors such as genetic abnormalities, testicular injury, or certain medical conditions that affect testicular function.
- Post-testicular Azoospermia:Post-testicular azoospermia involves issues that affect sperm transport or ejaculation after sperm production in the testes. This may include blockages or abnormalities in the epididymis, vas deferens, or ejaculatory ducts, leading to the absence of sperm in the ejaculate despite normal sperm production.
Symptoms of Azoospermia (Zero Sperm Count)
Azoospermia, or zero sperm count, often presents without noticeable symptoms on its own. However, underlying factors contributing to azoospermia may manifest with symptoms related to reproductive health or hormonal imbalances. Symptoms associated with azoospermia can include:
- Infertility.
- Changes in Sexual Function.
- Testicular Abnormalities.
- Hormonal Imbalances.
When to see a doctor?
It’s important to seek medical evaluation and guidance from a qualified healthcare provider if you have concerns about azoospermia or male infertility. Early detection, diagnosis, and treatment can improve the chances of successful management and conception.
Causes of Azoospermia (Zero Sperm Count)
Azoospermia, or zero sperm count, can result from various underlying factors that affect sperm production, transport, or ejaculation. Some common causes of azoospermia include:
- Obstructive factors.
- Non-obstructive factors.
- Hormonal imbalances.
- Genetic factors.
- Environmental factors.
- Idiopathic causes.
Diagnosis of Azoospermia (Zero Sperm Count)
The diagnosis of azoospermia, or zero sperm count, typically involves a series of tests and evaluations to determine the underlying cause and confirm the absence of sperm in the ejaculate. The diagnostic process may include:
- Medical History and Physical Examination: A healthcare provider will review the individual’s medical history, including any previous surgeries, medical conditions, medications, or exposures that may affect fertility. A physical examination may also be conducted to assess for any abnormalities in the reproductive organs.
- Semen Analysis: A semen analysis is the primary diagnostic test used to evaluate sperm count and quality. The individual will be asked to provide a semen sample through masturbation, which is then analyzed in a laboratory to assess sperm count, motility (movement), morphology (shape), and other parameters. A complete absence of sperm in the ejaculate confirms the diagnosis of azoospermia.
- Hormonal Testing: Blood tests may be performed to evaluate hormone levels, including testosterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin. Abnormal hormone levels can provide clues about potential underlying causes of azoospermia, such as hormonal imbalances or dysfunction of the hypothalamic-pituitary-gonadal axis.
- Imaging Studies: Imaging tests such as scrotal ultrasound may be performed to assess the structure and function of the reproductive organs, including the testes, epididymis, and vas deferens. Ultrasound can help identify abnormalities such as testicular atrophy, varicoceles (enlarged veins in the scrotum), or obstructive lesions.
- Genetic Testing: Genetic testing may be recommended to evaluate for chromosomal abnormalities or genetic mutations that can affect sperm production or function. This may include karyotype analysis, Y chromosome microdeletion testing, or genetic screening for specific gene mutations associated with azoospermia.
- Specialized Testing: In some cases, additional specialized tests or procedures may be performed to further evaluate the underlying cause of azoospermia. This may include testicular biopsy to assess testicular tissue for sperm production, or additional hormonal stimulation tests to evaluate testicular function.
- Comprehensive Evaluation: A comprehensive evaluation by a fertility specialist or reproductive endocrinologist is essential to determine the cause of azoospermia accurately. The results of diagnostic tests will help guide treatment decisions and management strategies tailored to the individual’s specific circumstances.
Treatments of Azoospermia (Zero Sperm Count)
The treatment of azoospermia, or zero sperm count, depends on the underlying cause and type of the condition. Treatment options may include:
- Surgical Interventions:
Obstructive Azoospermia: Surgical procedures may be performed to correct blockages or obstructions in the male reproductive tract. This may include procedures such as vasectomy reversal, epididymal or testicular sperm extraction (TESE), or reconstructive surgery to repair obstructed ducts.
Non-obstructive Azoospermia: Surgical interventions may be considered in certain cases of non-obstructive azoospermia, such as testicular sperm extraction (TESE) to retrieve sperm directly from the testes for use in assisted reproductive techniques.
- Hormonal Therapy:
Hormonal imbalances contributing to azoospermia may be treated with hormone replacement therapy or medications to restore normal hormonal levels and stimulate sperm production in the testes. Hormonal therapy may be effective in cases of hypogonadotropic hypogonadism or other hormonal disorders.
- Assisted Reproductive Techniques (ART):
Assisted reproductive techniques may be utilized to achieve pregnancy in couples affected by azoospermia. These techniques include:
In Vitro Fertilization (IVF): IVF involves fertilizing eggs with sperm in a laboratory setting and transferring resulting embryos into the uterus for implantation.
Intracytoplasmic Sperm Injection (ICSI): ICSI is a procedure where a single sperm is injected directly into an egg to facilitate fertilization. ICSI may be used in cases of severe male factor infertility, including azoospermia.
Testicular Sperm Extraction (TESE): TESE involves retrieving sperm directly from the testes through a surgical biopsy procedure. The retrieved sperm can then be used for ICSI in conjunction with IVF.
- Genetic Counseling and Testing:
Individuals with azoospermia associated with genetic abnormalities may benefit from genetic counseling and testing to assess the risk of passing on genetic disorders to offspring. Pre-implantation genetic testing (PGT) may be considered to screen embryos for genetic abnormalities before embryo transfer during IVF.
- Lifestyle Modifications:
Adopting a healthy lifestyle, including maintaining a balanced diet, regular exercise, avoiding tobacco, excessive alcohol consumption, and managing stress, may help optimize overall reproductive health and fertility outcomes.
- Alternative Treatments:
In some cases, alternative or experimental treatments may be considered, such as antioxidant supplementation, acupuncture, or traditional herbal remedies. However, the efficacy of these treatments for azoospermia remains uncertain and requires further research.
Why choose Shukan Hospital & IVF Centre in Ahmedabad for Azoospermia (Zero Sperm Treatment) treatment?
- Specialized Male Infertility Care: Our dedicated Male Infertility Clinic offers focused care for men facing fertility challenges like azoospermia.
- Advanced Diagnostic Technologies: We utilize cutting-edge diagnostic tools to thoroughly evaluate the root cause of azoospermia, ensuring precise treatment planning.
- Tailored Treatment Plans: Our expert team designs personalized treatment strategies based on your unique needs and medical history, maximizing success rates.
- Holistic Wellness Approach: We prioritize your overall well-being, integrating lifestyle modifications and stress management techniques into your treatment plan.
- Transparent Communication: We believe in clear, open communication, empowering you to make informed decisions about your fertility journey.
- Ongoing Support: Our compassionate team provides continuous support and follow-up care, ensuring you feel supported throughout your fertility experience.
- Patient-Centric Care: You’re more than just a patient to us – you’re a valued member of our fertility family, and we prioritize your comfort and satisfaction at every step.
Choose Shukan Hospital & IVF Centre for effective and compassionate care for Zero Sperm Count treatment in Ahmedabad.
Prevention of Azoospermia (Zero Sperm Count)
There are some lifestyle measures and preventive strategies that may help promote male reproductive health and reduce the risk of certain factors contributing to azoospermia:
- Maintain a Healthy Lifestyle.
- Avoid Excessive Heat Exposure.
- Limit Alcohol and Tobacco Use.
- Manage Stress.
- Protect Against Environmental Toxins.
- Practice Safe Sex.
- Regular Health Check-ups.
FAqs
Is IVF the only option if my partner has azoospermia?
No, IVF (in vitro fertilization) is not the only option. Depending on the cause of azoospermia, other treatments like surgical sperm retrieval (TESE or micro-TESE) with intracytoplasmic sperm injection (ICSI) or the use of donor sperm may also be considered.
Can I still get my partner pregnant if I have a zero sperm count?
Natural conception may not be possible, but assisted reproductive techniques like IVF with ICSI using surgically retrieved sperm or donor sperm can offer options for achieving pregnancy.
Will sperm come back after treatments of azoospermia?
It depends on the cause and effectiveness of treatment. In some cases, sperm may return after successful treatment, but ongoing management or alternative options may be needed.
What lifestyle changes can help manage azoospermia?
Maintaining a healthy weight, avoiding heat exposure to the genital area, limiting alcohol and tobacco use, managing stress, and minimizing exposure to toxins may help manage azoospermia.
Can azoospermia be prevented?
While not always preventable, adopting a healthy lifestyle and avoiding risk factors like tobacco and alcohol use may reduce the risk of certain causes of azoospermia.
How long does it take to cure azoospermia?
Duration varies based on the cause and treatment. Some cases may be treatable with surgery or hormone therapy, while others may require ongoing management or alternative options for conception.
What is a normal sperm count?
A normal sperm count typically ranges from 15 million to over 200 million sperm per milliliter of semen. Other factors like sperm motility and morphology also affect fertility. If concerned, consult a healthcare provider for evaluation and guidance.
